
A Parkinson's disease awareness and free consultation event is held at Beijing Tiantan Hospital of the Capital Medical University. (Photo: CFP)
Chinese scientists have identified a critical neural circuit that serves as the core target for Parkinson's disease. The study, published on Thursday in the journal Nature, reveals a missing link in how the brain coordinates movement and cognition, opening the door for highly precise, non-invasive treatments.
Solving the brain's 'action center' mystery
For years, Parkinson's disease was like a "dark maze" for researchers – they knew the brain was misfiring, but they couldn't find the exact location of the error. While typically associated with tremors, the disease is a whole-body disorder often involving sleep disturbances, cognitive decline, and autonomic issues like digestive problems.
The research, led by Professor Liu Hesheng of Changping Laboratory in Beijing alongside specialists from Peking and Tsinghua universities, involved analyzing over 800 clinical datasets. The team locked onto a core functional circuit called the Somato-Cognitive Action Network (SCAN).
Acting like the brain's "action command center," the SCAN connects six deep brain regions, including the thalamus, to the cerebral cortex. While scientists previously knew these deep regions were involved in Parkinson's, they didn't know the exact locations where they interface with the brain's surface – a major blind spot that this study has finally mapped.
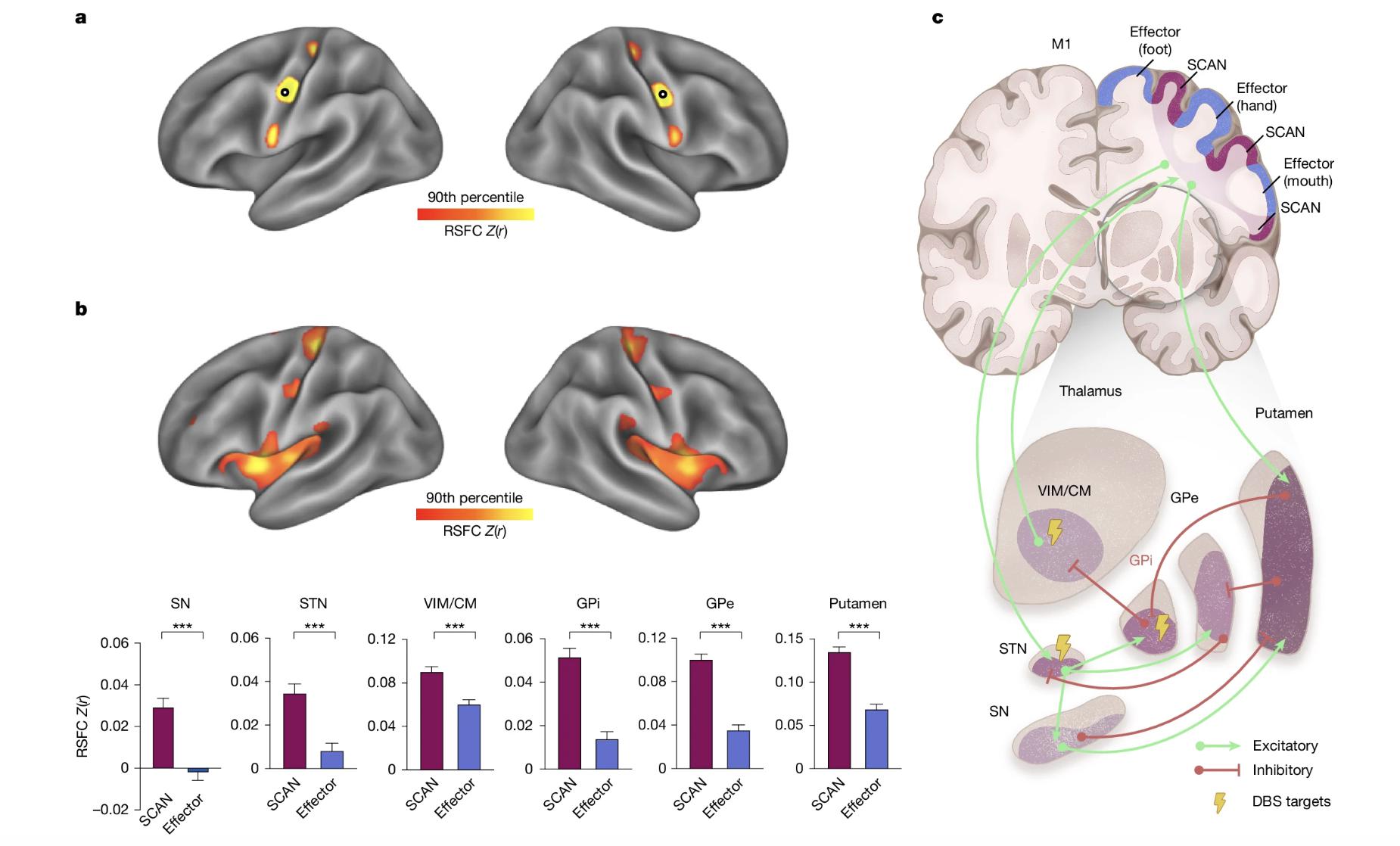
Screenshot of a diagram mapping the cortical functional connectivity of six subcortical regions critical in Parkinson's disease. (Photo: Nature)
Resolving the 'signal overload'
The study found that in Parkinson's patients, this command center is in a state of "hyperconnectivity." This means the neural connections between the deep brain and the surface are pathologically strengthened, leading to a breakdown in communication.
This malfunction can be compared to a commander trying to process dozens of urgent phone calls simultaneously. It results in a state of "signal overload," causing the classic physical symptoms of the disease – the "shaky, slow and stiff" movements – as well as cognitive interference.
The researchers found that existing treatments, such as oral medications and deep-brain stimulation (DBS), already work by modifying this specific circuit. By mapping the SCAN, scientists now have a clear guide to improve these therapies.

Stanford neurologist Gaurav Chattree monitors a patient receiving adaptive deep-brain stimulation, an FDA-approved personalized Parkinson's treatment, at the Stanford Neuroscience Health Center, California, United States, March 21, 2025. (Photo: CFP)
New hope for non-invasive therapy
The identification of this target has immediate practical applications. The team has developed a new generation of brain circuit stimulation systems capable of millimeter-level precision.
Unlike traditional treatments that often target general motor areas, this system focuses specifically on the SCAN. After two weeks of treatment, the treatment success rate reached 55.5 percent, which is double that of traditional stimulation targets.
This discovery also provides patients with effective non-invasive options, potentially reducing the reliance on heavy medication or invasive surgeries like DBS.
A new framework for treatment
By proving that the SCAN is at the heart of the disease, the study suggests that Parkinson's should be viewed as a "circuit disorder" rather than just a movement problem.
This shift in understanding allows doctors to move away from treating vague symptoms and toward fixing a specific pathological pathway. While further clinical rollout is required, this research provides a clear roadmap for more personalized and effective neuromodulation therapies, offering an advancement in the long-term management of the disease.


