Editor's note: Lung cancer is the leading cause of cancer-related deaths worldwide, with an estimated 1.8 million deaths in 2020. The incidence and mortality rates of lung cancer in China are both higher than the world average. CGTN spoke to China's leading thoracic surgery expert Zhou Qinghua, a professor with the Lung Cancer Center of West China Hospital of Sichuan University. He has long been engaged in the surgical diagnosis and treatment of thoracic tumors, specializing in lung cancer surgery and multidisciplinary comprehensive therapy.

(Photo: VCG)
After more than five decades in medicine, the scalpel of Professor Zhou Qinghua of West China Hospital, Sichuan University, has produced many miracles.
He pioneered the "cardiac displacement tracheal reconstruction" technique, extending the resectable tracheal length from the internationally accepted limit of 4 cm to 9.5 cm. He has enabled patients with advanced lung cancer, once deemed hopeless, to return to normal life. The Phase III lung cancer surgical data contributed by his team has even rewritten international treatment guidelines.
Chinese physicians represented by Zhou are writing a Chinese chapter in the global story of lung cancer diagnosis and treatment with their innovation and dedication. Yet, for Professor Zhou, the origin of all this innovation is simple: The patient's interests are above everything else.
The evolution of treatment
Lung cancer starts when some cells in the lung tissue reproduce out of control. This creates a crowded mass of abnormal cells called a tumor. The tumor can grow into and block the tubes that carry air or invade nearby blood vessels. Cancer cells can also break off from the main tumor and travel to other parts of the body to start new colonies, disrupting organ function.
To stop these cancer cells from growing and traveling, a surgeon usually first cuts out the cancer and some of the healthy tissue around it to make sure they get all the rebel cells.
The past decade has witnessed the rapid development of lung cancer treatment, with models shifting from a single path to multi-disciplinary treatment (MDT).

(Photo: VCG)
Targeted therapies attack only cancer cells harboring specific genetic mutations, thereby maximizing the protection of normal tissues. In 2003, a small molecule drug, gefitinib, was launched and is used to treat non-small cell lung cancer (NSCLC).
"Targeted drugs for both classic and rare mutations now have first, second, and third generations, with fourth-generation drugs soon to be launched," Zhou said.
Currently, China has more marketed targeted drugs for both classic and rare mutations than Western countries. Zhou pointed out, "Besides imported targeted drugs, China also has domestically developed, original drugs with independent intellectual property rights."
Immunotherapy is a type of cancer treatment that utilizes the body's immune system to identify and attack cancer cells. It works by stimulating or enhancing the immune response, allowing the body to better recognize and destroy cancerous cells.
In 2014, the PD-1 (programmed cell death protein 1) inhibitor pembrolizumab was approved by the U.S. FDA, bringing a new breakthrough in lung cancer treatment. In 2018, the immunotherapy drug was officially launched in China.
This shifted lung cancer treatment from traditional histological classification to molecular typing guided by relevant driver genes. Patients with positive driver genes receive molecular targeted therapy as the core of MDT, while those with negative driver genes are primarily treated with chemotherapy combined with immunotherapy.

(Photo: VCG)
Even more exciting in recent years is the emergence of the sandwich treatment model – a comprehensive strategy that includes preoperative neoadjuvant immunotherapy combined with chemotherapy, surgical resection and postoperative adjuvant immunotherapy.
This approach aims to activate the immune system before surgery to shrink tumors and to reduce the stage of cancer, to achieve radical resection during surgery and to continuously eliminate minimal residual disease after surgery. So far, studies in China and abroad have shown positive results for survival rate.
A case that redefined 'impossible'
In 2021, a patient with advanced lung adenocarcinoma traveled from the UK to Chengdu, the capital of southwest China's Sichuan Province. The patient presented with a right lower lobe adenocarcinoma accompanied by bilateral lung metastases, bilateral pleural metastases with massive effusion and pericardial metastasis with tamponade syndrome.
Many advised giving up, but Zhou didn't when the patient found him. After going through emergency pericardiocentesis and targeted therapy combined with chemotherapy, the patient finally got the opportunity to have surgery after the MDT discussion. She also received treatment of postoperative adjuvant targeted therapy for three years.
Today, over five years later, she lives and works normally like anyone else, having settled in Chengdu to teach English.
From simple resection to functional reconstruction
Zhou's pioneering "thoracic oncologic reconstructive surgery" has advanced thoracic surgery from traditional resection to organ and functional reconstruction.
According to Zhou, the core elements of this theory include ensuring complete en bloc tumor resection, completely en bloc resecting tissues and organs invaded by the tumor, using the patient's own tissues or artificial materials to reconstruct the resected organs, and ensuring the reconstructed organs can restore normal function.
Most notably, he created the "cardiac displacement tracheal reconstruction" technique, which has been highly recognized and praised by many experts around the world.
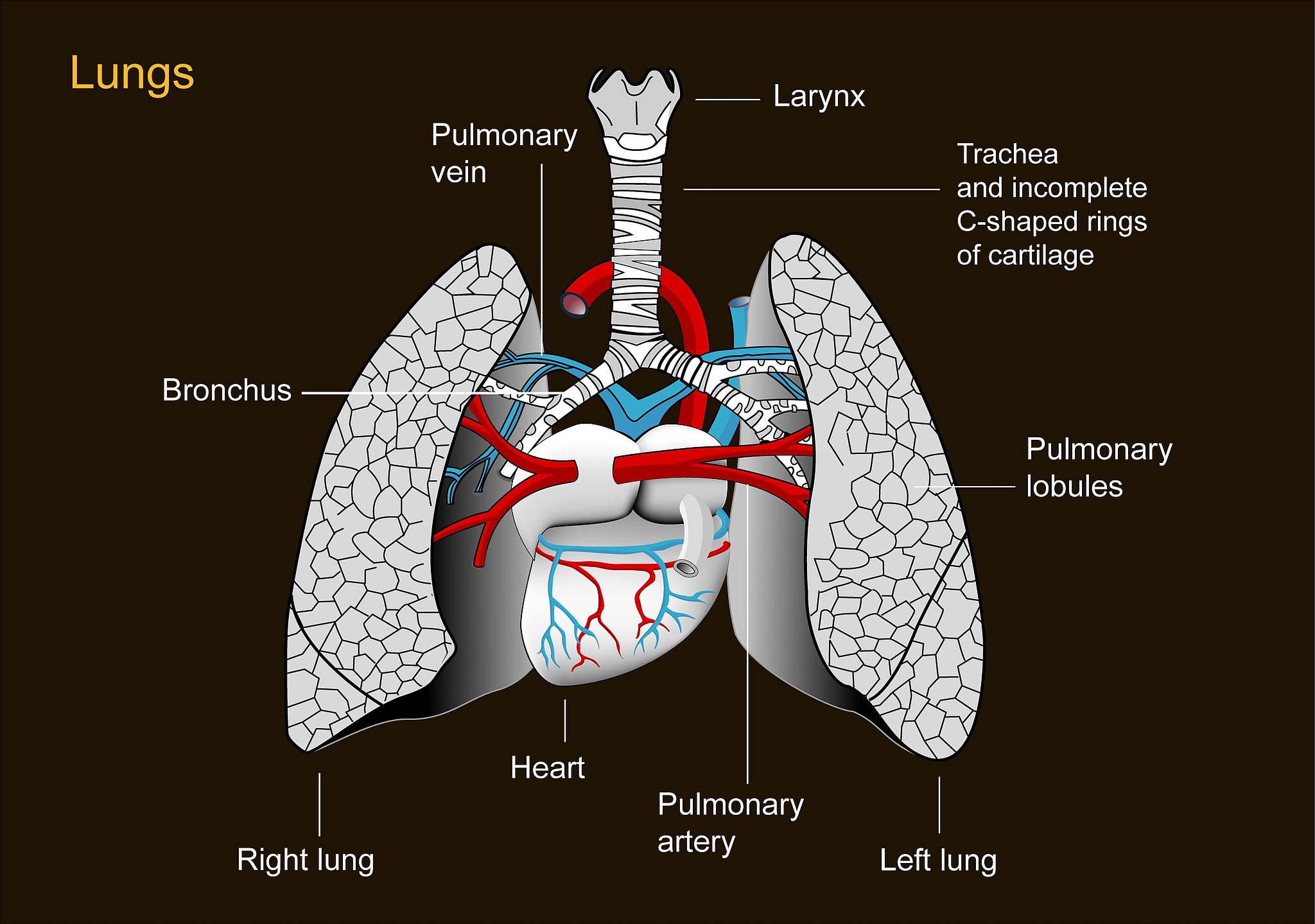
Illustration of human lungs and heart. /VCG
The total length of the human trachea is only 12-13 cm. Because the trachea connects to both lungs via the main bronchi and to the heart via the pulmonary arteries and veins, the heart is relatively fixed. Thus, the globally accepted maximum resectable tracheal length was 4-5 cm.
"I thought of resecting the pericardium on one side, freeing the vena cava and the main pulmonary artery, allowing the lung and heart to shift upward as a unit by 7-9 cm," Zhou recalled.
Since 1992, Zhou and his team have completed over 400 surgeries for patients with unresectable tracheal tumors or lung cancer invading the trachea, with the longest resected tracheal segment exceeding 9.5 cm.
International cooperation
"We have broad prospects for future international cooperation, especially in basic medicine and translational medicine," Zhou said, acknowledging the gap between China and Western countries in basic research and the standardization and normalization of clinical lung cancer diagnosis and treatment.
"In the past, we learned from the West how to conduct clinical trials for new drugs. Later, we ran alongside them. Now, we are beginning to lead some lung cancer clinical studies," Zhou traced this progression.
"China has a huge lung cancer population base, allowing real-world clinical studies on the efficacy of anti-lung cancer drugs to be completed very quickly," Zhou said. Global multi-center clinical researchers prefer collaborating with Chinese doctors because "it takes them five years to enroll patients, while we can complete enrollment in one year."


